If you’ve been silently dealing with itching, burning, or bleeding during bowel movements, you’re not alone. Millions of people experience hemorrhoids, yet most suffer in silence—too embarrassed to talk about it, too overwhelmed to understand what’s really going on. For some, it starts as a minor annoyance. For others, it becomes a recurring nightmare. Either way, the uncertainty can feel just as painful as the condition itself.
But it doesn’t have to stay that way. Whether you’re facing your first flare-up or have lived with hemorrhoids for years, this guide is here to finally help you understand what’s happening to your body—and what you can do about it. Backed by medical research and real patient insights, we’ll walk you through the causes, types, symptoms, and most importantly, the hemorrhoid treatment options that actually work—all explained in a clear, honest, and jargon-free way.
Imagine knowing what to do the next time you feel that all-too-familiar sting—or better yet, preventing it altogether. By the end of this guide, you won’t just understand hemorrhoids; you’ll know which hemorrhoid treatments are right for you, and how to take back control with confidence. Let’s begin.
What Are Hemorrhoids?
Let’s start with the basics: what exactly are hemorrhoids? Despite how common they are, many people have no idea what’s really happening when they’re told they have hemorrhoids—or worse, when they diagnose themselves after Googling their symptoms at 2 a.m.
Hemorrhoids are actually normal anatomical structures—soft, cushion-like veins in the lower rectum and anus that help you control bowel movements. It’s only when these veins become swollen or inflamed that they start causing problems. This swelling can lead to pain, itching, bleeding, or even a noticeable lump, especially during or after using the bathroom.
In other words, hemorrhoids aren’t some strange disease—they’re a natural part of your body that sometimes get irritated. And once you understand why that happens, it becomes a lot easier to find relief and take control.
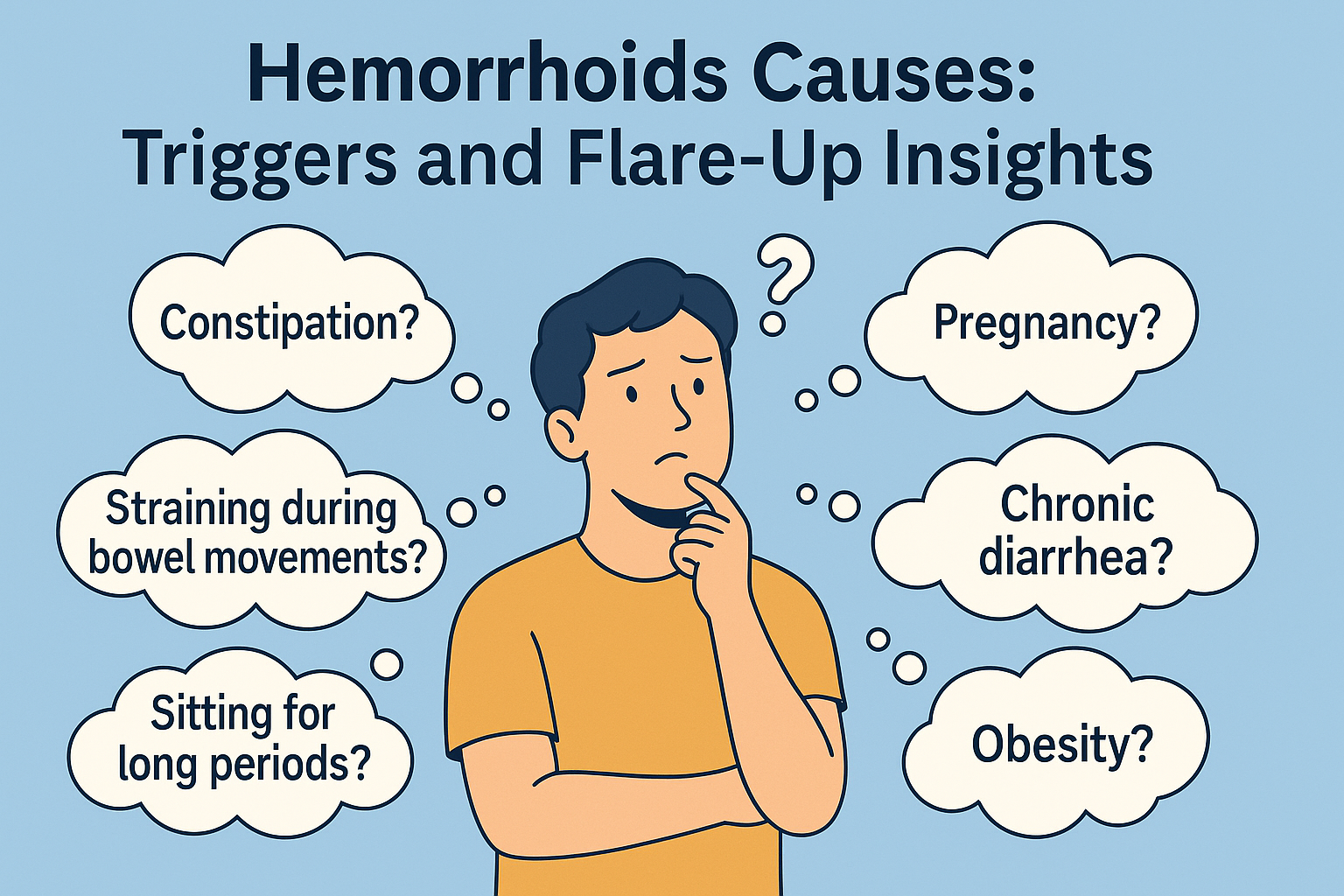
Main Causes of Hemorrhoids
Medically speaking, hemorrhoids are swollen and inflamed veins in the rectum or anus. Think of them like varicose veins, but in a much more sensitive area. Everyone has hemorrhoidal tissue—it’s part of your anatomy and plays a role in keeping bowel movements controlled. It’s only when these blood vessels become stretched, irritated, or inflamed that they’re considered a problem.
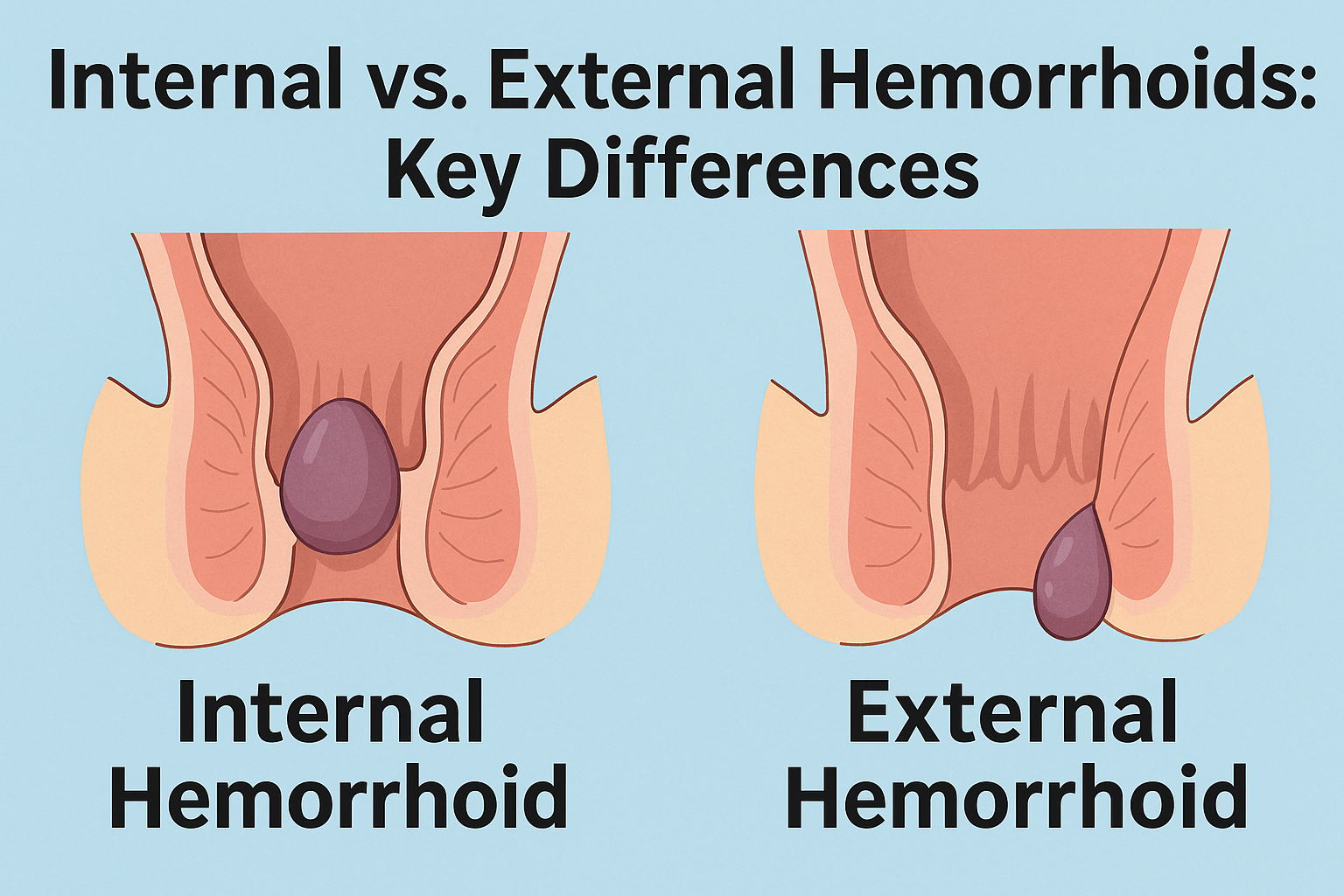
There are two main types: internal hemorrhoids, which develop inside the rectum and are often painless but may cause bleeding, and external hemorrhoids, which form under the skin around the anus and can cause itching, pain, or swelling. Sometimes, a clot forms in an external hemorrhoid, creating what’s known as a thrombosed hemorrhoid—a painful, hard lump that often feels worse when sitting or passing stool.
Types of Hemorrhoids
Understanding the difference between internal and external hemorrhoids is more than just medical trivia—it’s the key to choosing the right treatment and knowing when to seek help. Since they affect different parts of the anal canal, they show up in different ways and respond to different types of care. In the next section, we’ll take a closer look at the main types of hemorrhoids, how to recognize them, and what makes each one unique in symptoms and severity.
Common Symptoms of Hemorrhoids
Once hemorrhoids become swollen or irritated, they begin to make their presence known—and often not in subtle ways. Some people notice a streak of bright red blood on the toilet paper, while others experience persistent itching, discomfort when sitting, or even a painful lump near the anus. These symptoms can range from mildly annoying to seriously disruptive, and they often come and go depending on your habits, diet, and daily routine.
When to Seek Medical Help
It’s easy to dismiss hemorrhoid symptoms as something you can just “deal with,” especially when they seem to come and go. But not all discomfort should be ignored. If you’re experiencing rectal bleeding that lasts more than a few days, significant pain while sitting or during bowel movements, or any changes in your symptoms that seem unusual or severe, it’s time to speak with a doctor. In rare cases, symptoms that look like hemorrhoids may be signs of something more serious, such as an anal fissure or even colorectal cancer.
Who Gets Hemorrhoids? Risk Groups and Solutions
You might think hemorrhoids only affect older adults, but the truth is they can strike almost anyone. Common high-risk groups include:
- Office Workers: Sitting for 8+ hours a day increases pressure on rectal veins.
- Pregnant Women: Growing uterus puts extra abdominal pressure on pelvic blood vessels.
- Weightlifters & Athletes: Repeated straining from heavy lifts can aggravate veins.
- Chronic Constipation Sufferers: Straining to pass hard stools is a top trigger.
- Phone-Scrolling “Toilet Tourists”: Spending extra minutes on the throne adds unnecessary stress.
While genetics can play a role, lifestyle factors are often the biggest culprits. The good news? Once you know your personal risk, there are simple steps—and targeted products—you can use to reduce flare-ups and stay more comfortable every day.
Ready to Level Up Your Prevention?
Don’t wait for your next flare-up to strike. Explore our in-depth guide to the 12 Best Hemorrhoid Supplements for 2025—featuring powerful venotonic formulas, anti-inflammatory herbs, and digestive support blends designed to target hemorrhoids from the inside out. Whether you’re dealing with early symptoms or aiming to prevent future discomfort, these supplements offer a proactive, natural approach to staying flare-free.
👉 See the 12 Best Hemorrhoid Supplements of 2025 »
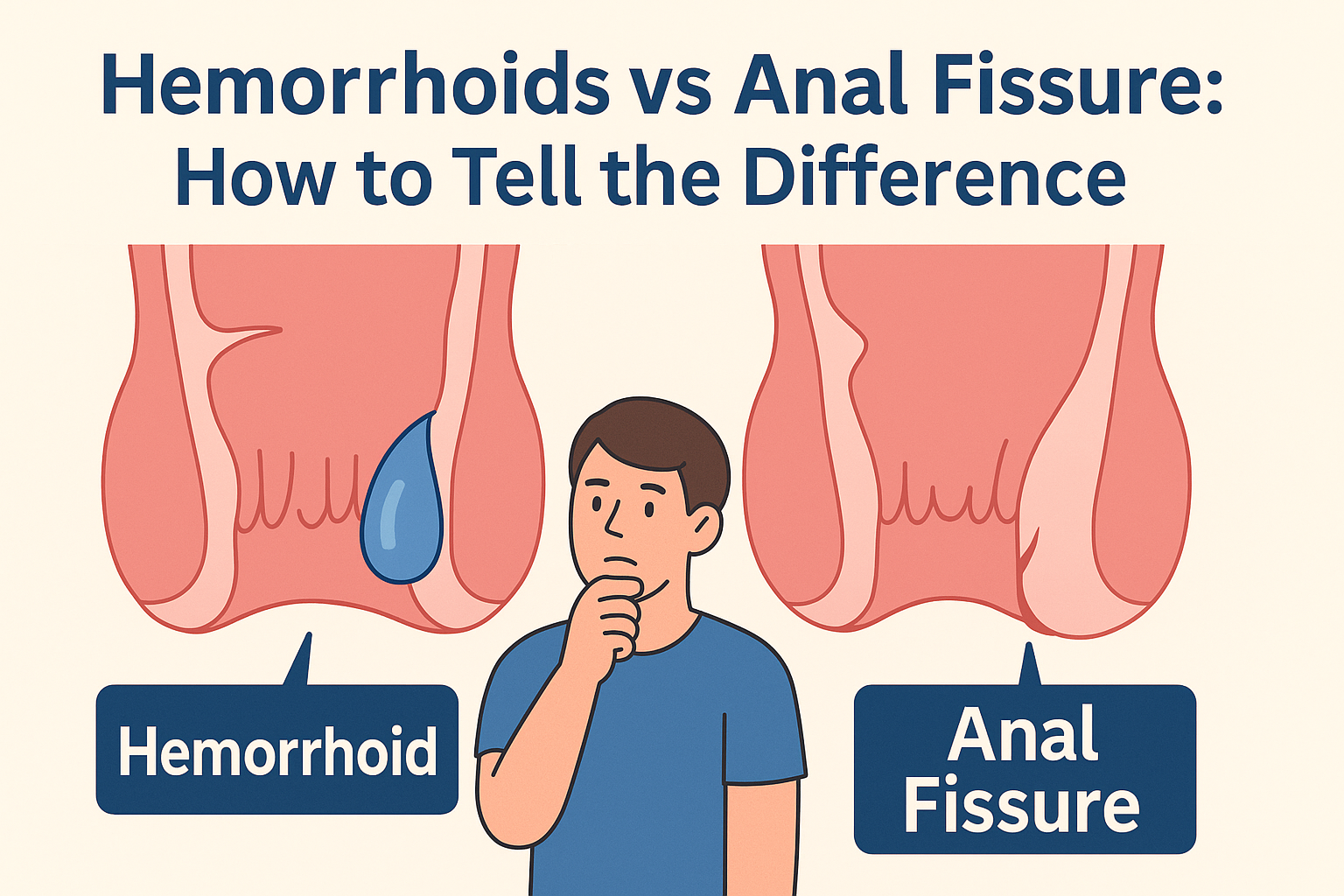
Hemorrhoids vs. Other Anal Conditions
Not every itch, lump, or spot of blood means you have hemorrhoids. In fact, several other anal and rectal conditions can cause similar symptoms—but require very different treatments. Anal fissures, which are small tears in the lining of the anus, can feel sharp and sting during bowel movements. Rectal prolapse involves a portion of the rectum pushing outside the body, often mistaken for a prolapsed hemorrhoid. And in more serious cases, rectal bleeding could signal colorectal cancer. That’s why knowing the difference isn’t just helpful—it’s critical.
How Hemorrhoids Are Diagnosed
If the idea of seeing a doctor for hemorrhoids makes you nervous, you’re not alone. Many people delay getting help because they’re embarrassed or unsure what to expect. But the reality is that diagnosing hemorrhoids is usually quick, simple, and often non-invasive. Most doctors start with a brief conversation about your symptoms and lifestyle. From there, they may perform a visual exam or, in some cases, a digital rectal exam or use a small instrument called an anoscope to look inside the rectum. These procedures are typically painless and over in minutes—but they can make a huge difference in getting the right treatment and ruling out more serious issues.
👉 For a detailed breakdown of diagnostic methods and treatment plans, you can also refer to the Mayo Clinic’s hemorrhoid treatment overview.
Common Misconceptions About Hemorrhoids
Despite how common hemorrhoids are, myths and misunderstandings about them are everywhere. Maybe you’ve heard that only old people get them, or that they always cause pain, or even that hemorrhoids can turn into cancer. These beliefs aren’t just inaccurate—they can prevent people from seeking proper treatment or taking preventive steps. The truth is, hemorrhoids affect people of all ages, and while they can be painful, they’re often painless at first. Clearing up these misconceptions can help you approach your symptoms with more confidence—and less fear.
Your First Steps If You Suspect Hemorrhoids
So what should you do if you think you have hemorrhoids? The good news is that most cases—especially early ones—can be managed at home with a few simple steps. Start by drinking more water, adding fiber to your diet, and avoiding straining during bowel movements. Warm sitz baths, gentle cleansing with unscented wipes, and avoiding long periods on the toilet can also make a big difference. And if discomfort is already interfering with your daily life, over-the-counter creams, suppositories, and wipes may offer fast relief.
If you’re unsure which products are safe and effective, don’t worry—we’ve reviewed the best options for you. 👉 See our top-rated hemorrhoid relief products here
👉 You can also download the Mayo Clinic’s official patient handout on hemorrhoids (PDF) for a quick reference on symptoms, causes, and self-care strategies.
Conclusion: You Don’t Have to Suffer in Silence
Hemorrhoids are more common—and more manageable—than most people realize. From understanding what they are and why they happen, to recognizing symptoms and knowing when to seek help, you now have a clear foundation to make informed decisions about your health. Whether you’re dealing with mild irritation or ongoing discomfort, taking the right steps early can make a world of difference.
We know how confusing and isolating this topic can feel. That’s why we’re committed to providing straightforward, evidence-based, and compassionate guidance—written for real people, not just medical professionals. If this guide helped you feel more confident and less alone, then we’ve done our job.
Frequently Asked Questions
Will hemorrhoids go away on their own?
Yes, mild cases of hemorrhoids can go away on their own with lifestyle changes such as increased fiber intake, better hydration, and avoiding straining during bowel movements. However, persistent or severe cases may require treatment.
How do you fix hemorrhoids?
Treatment depends on severity. Home remedies include sitz baths, high-fiber diets, and over-the-counter creams. In more advanced cases, medical procedures like rubber band ligation or infrared coagulation may be recommended.
Why do hemorrhoids happen?
Hemorrhoids develop when pressure builds in the lower rectum. Common causes include constipation, prolonged sitting, straining during bowel movements, pregnancy, and obesity.
Can hemorrhoids heal?
Yes, many hemorrhoids can heal with conservative care. Healing time varies based on type (internal vs. external), severity, and whether the patient makes consistent lifestyle changes.
How can I treat hemorrhoids myself?
Start with fiber-rich foods, drink plenty of water, avoid sitting too long, and take warm sitz baths. Use fragrance-free wipes and apply soothing creams containing witch hazel or lidocaine if needed.