Hemorrhoids are a common medical condition affecting millions of people worldwide. By age 50, about half the population has experienced one or more of the classic symptoms of hemorrhoids, which include rectal pain, itching, bleeding, and possibly prolapse. Proper care for hemorrhoids begins with understanding the different types and their unique symptoms. Understanding the difference between internal and external hemorrhoids is crucial for proper diagnosis and treatment. This article explores the key differences between these two types and provides information on their symptoms, treatment options, and hemorrhoids how can be effectively managed at home or when medical intervention is necessary.
What Are Hemorrhoids?
Hemorrhoids, sometimes called piles, are swollen veins in the anal and rectal area. They’re similar to varicose veins that can develop in the legs. While everyone has hemorrhoidal tissue as part of their normal anatomy, the term “hemorrhoids” refers to when these blood vessels become enlarged, inflamed, or symptomatic.
Difference #1: Location
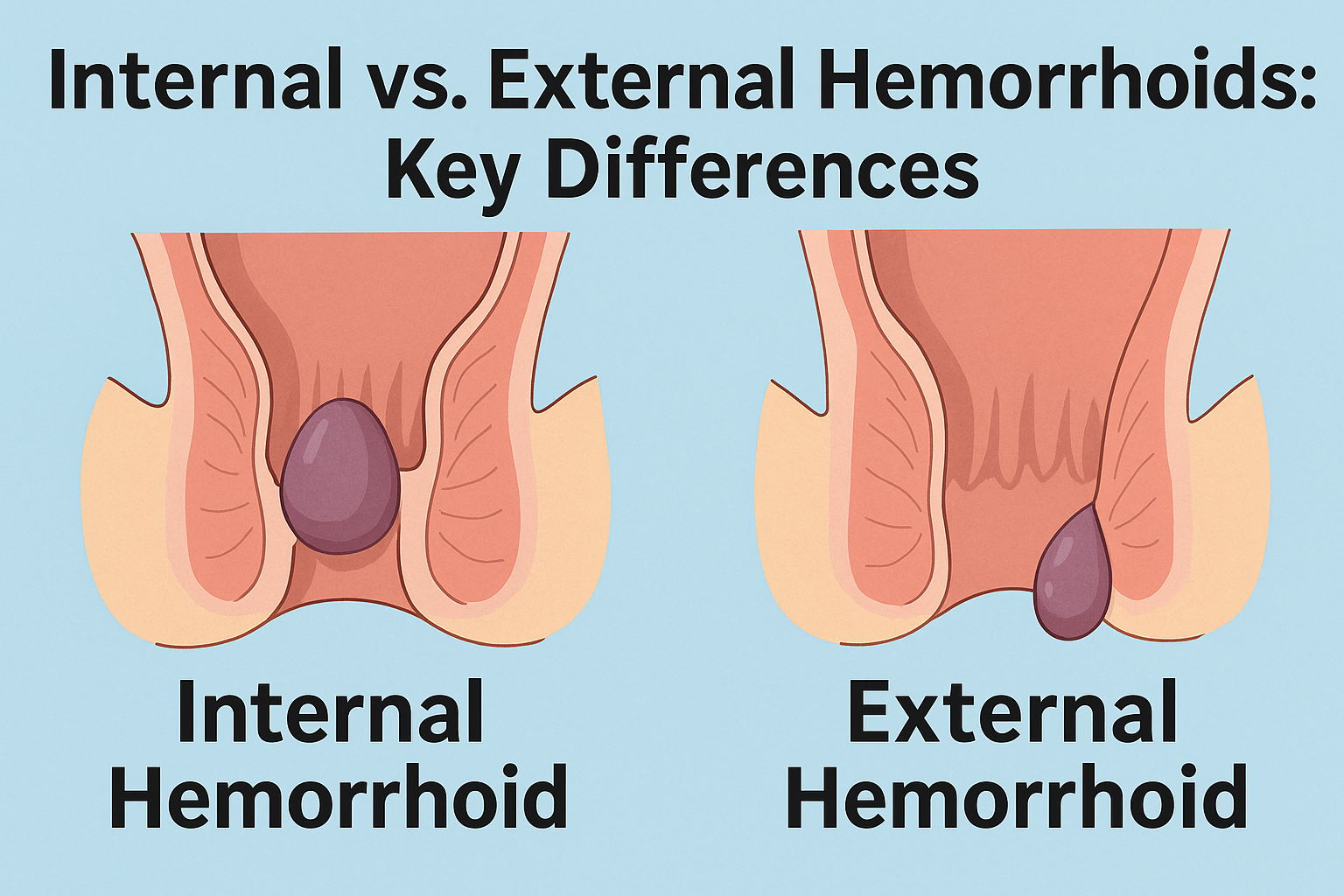
The most fundamental difference between internal and external hemorrhoids is their location.
Internal hemorrhoids develop inside the rectum, above what doctors call the dentate line. This tissue boundary marks where the rectum transitions to the anal canal. Because this area has fewer pain-sensing nerves, internal hemorrhoids often go unnoticed until they bleed or prolapse.
External hemorrhoids form under the skin around the anal opening, below the dentate line. This area contains many more pain-sensing nerves, which is why external hemorrhoids typically cause more discomfort and are more easily detected.
Difference #2: Symptoms
The symptoms of internal and external hemorrhoids differ significantly due to their locations.
Internal hemorrhoid symptoms:
- Painless bright red bleeding during bowel movements
- Mucus discharge
- A feeling of incomplete evacuation
- Usually painless unless they prolapse
- May cause anal itching or irritation
External hemorrhoid symptoms:
- Pain or discomfort, especially when sitting
- Itching or irritation in the anal region
- Visible swelling around the anus
- A hard, possibly painful lump near the anus
- More noticeable pain during bowel movements
Difference #3: Classification and Severity Stages
Internal and external hemorrhoids progress differently and use different classification systems.
Internal hemorrhoids are classified into four grades based on their level of prolapse:
- Grade 1: No prolapse. These hemorrhoids remain inside the rectum and are usually only detected through examination or when they cause bleeding.
- Grade 2: Prolapse during bowel movements or straining but retract on their own.
- Grade 3: Prolapse during physical activities and require manual pushing back inside.
- Grade 4: Permanently prolapsed and cannot be pushed back in, often requiring medical intervention.
External hemorrhoids don’t follow the same grading system. Instead, they’re typically categorized as:
- Uncomplicated external hemorrhoids
- Thrombosed external hemorrhoids (containing a blood clot)
- Resolved external hemorrhoids (which may leave skin tags)
Difference #4: Complications and Associated Conditions
Internal and external hemorrhoids can develop different complications if left untreated.
Internal hemorrhoid complications:
- Prolapse: As mentioned above, internal hemorrhoids can protrude through the anal opening.
- Strangulation: When a prolapsed hemorrhoid’s blood supply is cut off by anal muscles, causing severe pain and tissue death.
- Anemia: In rare cases, chronic bleeding from internal hemorrhoids can lead to iron deficiency anemia.
External hemorrhoid complications:
- Thrombosis: External hemorrhoids can develop blood clots, causing severe pain, swelling, and a hard lump. The skin over the hemorrhoid may appear blue due to the clot.
- Skin tags: After an external hemorrhoid resolves, it may leave behind excess skin that can cause hygiene issues or discomfort.
- Infection: Though rare, external hemorrhoids can become infected if the skin breaks.
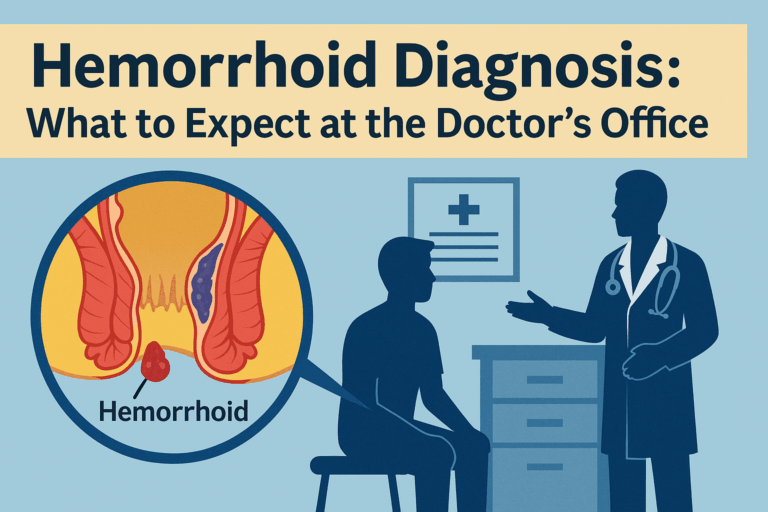
Diagnosis and When to Seek Medical Help
While most hemorrhoids aren’t dangerous, certain symptoms warrant medical evaluation. You should consult a healthcare provider if you experience persistent bleeding, severe pain unrelieved by home treatments, a prolapsed hemorrhoid that cannot be pushed back, symptoms that don’t improve after a week, or signs of infection like fever or increasing pain.
Doctors typically diagnose hemorrhoids through a physical examination. External hemorrhoids are visible upon inspection, while internal hemorrhoids may require a digital rectal examination or anoscopy for proper assessment. For individuals over 45 or those with risk factors, more extensive examination like colonoscopy may be recommended to rule out other causes of rectal bleeding such as colorectal cancer.
Conclusion
Understanding the differences between internal and external hemorrhoids is essential for effective management and treatment. Though both types stem from the same cause—swollen blood vessels—they differ significantly in location, symptoms, classification systems, and potential complications. Most hemorrhoid cases respond well to conservative treatments and lifestyle modifications, but more severe cases may require medical intervention.
Don’t let embarrassment prevent you from seeking help if you’re experiencing rectal bleeding or persistent discomfort. Early diagnosis leads to more effective treatment and can prevent complications from developing. With proper care and preventive measures, most people can find relief from hemorrhoids and maintain better anal health.
How long do external hemorrhoids last?
External hemorrhoids typically last between a few days to several weeks, depending on their severity and the treatment approach. Small hemorrhoids may clear up without any treatment within a few days, while large external hemorrhoids may take longer to heal and cause significant pain and discomfort.
For mild cases with minimal symptoms, recovery often occurs within a week with basic home care like sitz baths and over-the-counter treatments. Moderate cases usually improve within 1-2 weeks with consistent treatment. However, thrombosed hemorrhoids (those containing blood clots) may take 2-3 weeks to fully resolve, with the most severe pain occurring in the first 48-72 hours.
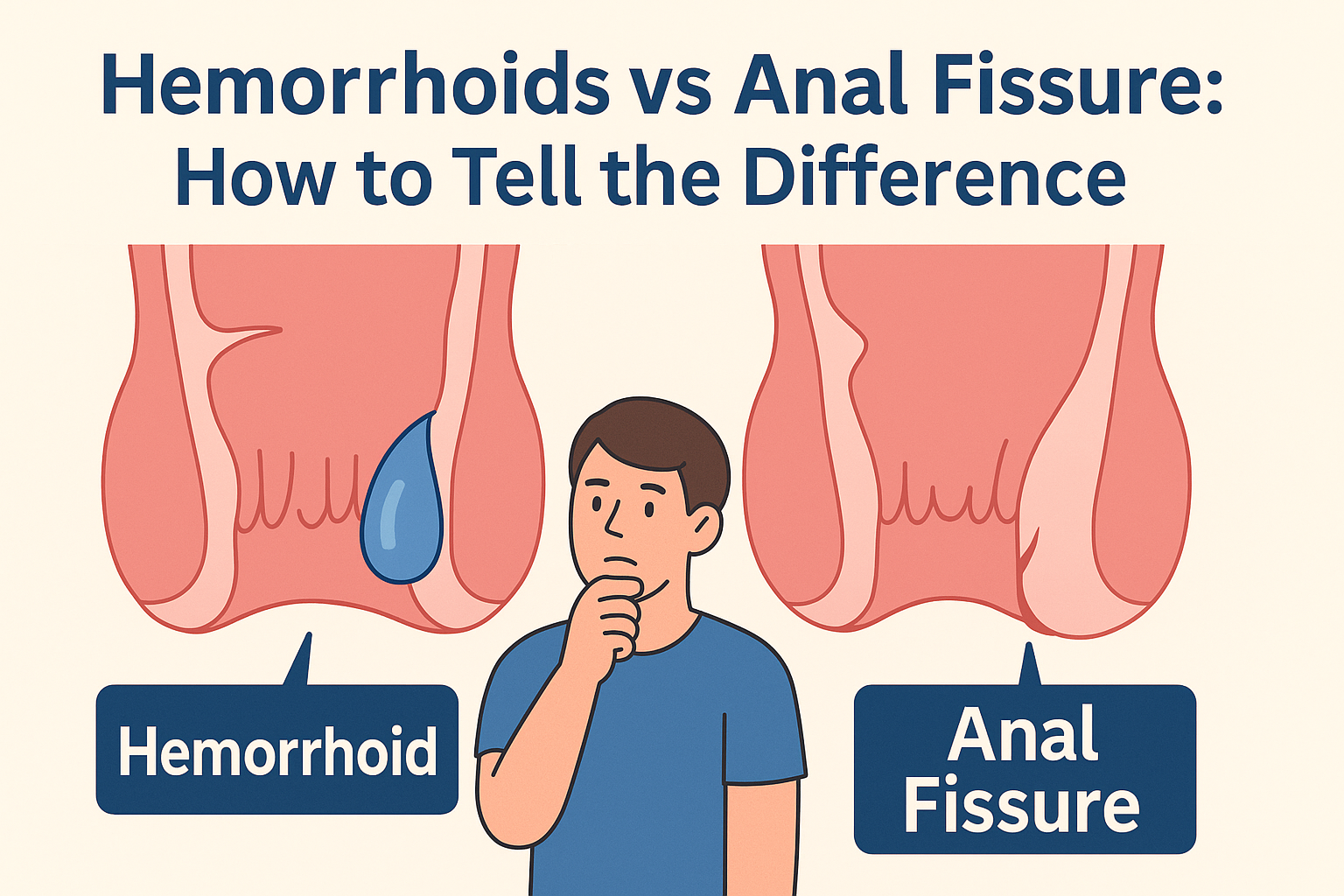
What can be mistaken for a hemorrhoid?
Several conditions can be mistaken for hemorrhoids due to similar symptoms. Anal fissures, which are tears in the lining of the anal canal, often cause severe pain during bowel movements that may linger for hours – more intense than typical hemorrhoid pain. Both colorectal and anal cancers can cause rectal bleeding or anal lumps similar to hemorrhoids, making medical evaluation crucial for persistent symptoms. Colonic polyps can cause bleeding without pain, mimicking internal hemorrhoids, while inflammatory bowel conditions like ulcerative colitis may cause bloody stools with additional symptoms like fever or abdominal pain. Other conditions sometimes confused with hemorrhoids include perianal abscesses, skin tags, and pruritus ani (intense anal itching).